Diabetes Distress
Living with an unpredictable health condition can be extremely challenging, so it is understandable for people to experience some difficult thoughts and feelings about their diabetes.
Watch the following video to learn more about distress and burnout:
See how people living with diabetes say that the challenges of juggling their condition alongside the demands of day-to-day life can, at times, make them feel:
- Overwhelmed with what needs to be learned/done to live well with diabetes
- Frustrated or angry at diabetes and what it asks of them
- Guilty about their numbers, e.g. HbA1c
- Sadness comparing life now to before diabetes came along
These are some possible emotions linked to living with diabetes, and are examples of something called “diabetes distress”. They can last from a few seconds through to minutes, hours, or even days and weeks at a time. Diabetes distress is not another diagnosis, it is a rational and common emotional response to the demands of living with a long-term health condition.
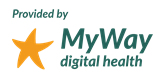
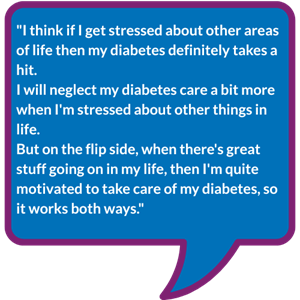
Below you can see how Faizah and Christy cope with diabetes distress:


The level of diabetes distress people experience can vary over time, and may be more severe during periods of stress.
A helpful analogy is the “stress bucket”. Imagine a bucket you carry around that gradually fills up every time you experience something difficult or stressful. Everyday tasks like work, finances, and chores, can also add to your bucket. When you go through a particularly difficult time, it is normal for your bucket to feel quite full – it can even feel like the bucket is overflowing.
During these periods, it can be harder to think about, and make time for diabetes self-care, which can increase the chance of experiencing diabetes distress.
Where can I get support if I am worried about diabetes distress or burnout?
|
|
|
|
|
There are also a number of strategies you can try yourself to help with overcoming diabetes burnout.
Further support
To learn more about emotional well-being and Type 1 diabetes, explore the free BERTIE Emotional Wellbeing module available on the BERTIE website.
This resource was created by Dr Lindsey Rouse, a clinical psychologist working in the Diabetes and Endocrine Centre at Royal Bournemouth Hospital (UHD NHS Trust) and part of the BERTIE team.